A clean bill of health: the role of environmental monitoring in veterinary practice
The start of a new year offers an ideal opportunity to embrace fresh beginnings and implement meaningful changes. Whether your New Year’s resolutions are well underway or have already fallen by the wayside, January serves as a timely reminder to refocus priorities. In veterinary practice, this is the perfect moment to focus on hygiene, a critical area that has a direct impact on not just patient care and clinical outcomes, but staff safety too.
How clean is your practice?
Infection control is an essential component of managing a veterinary practice. Nosocomial or hospital acquired infections (HAIs) are a known and recognised risk of hospital care, whether in human or veterinary medicine. In fact, in human healthcare, HAIs are not only associated with increased length of hospital stays, increased costs and morbidity, but also feature in the top ten causes of death among hospitalised patients.
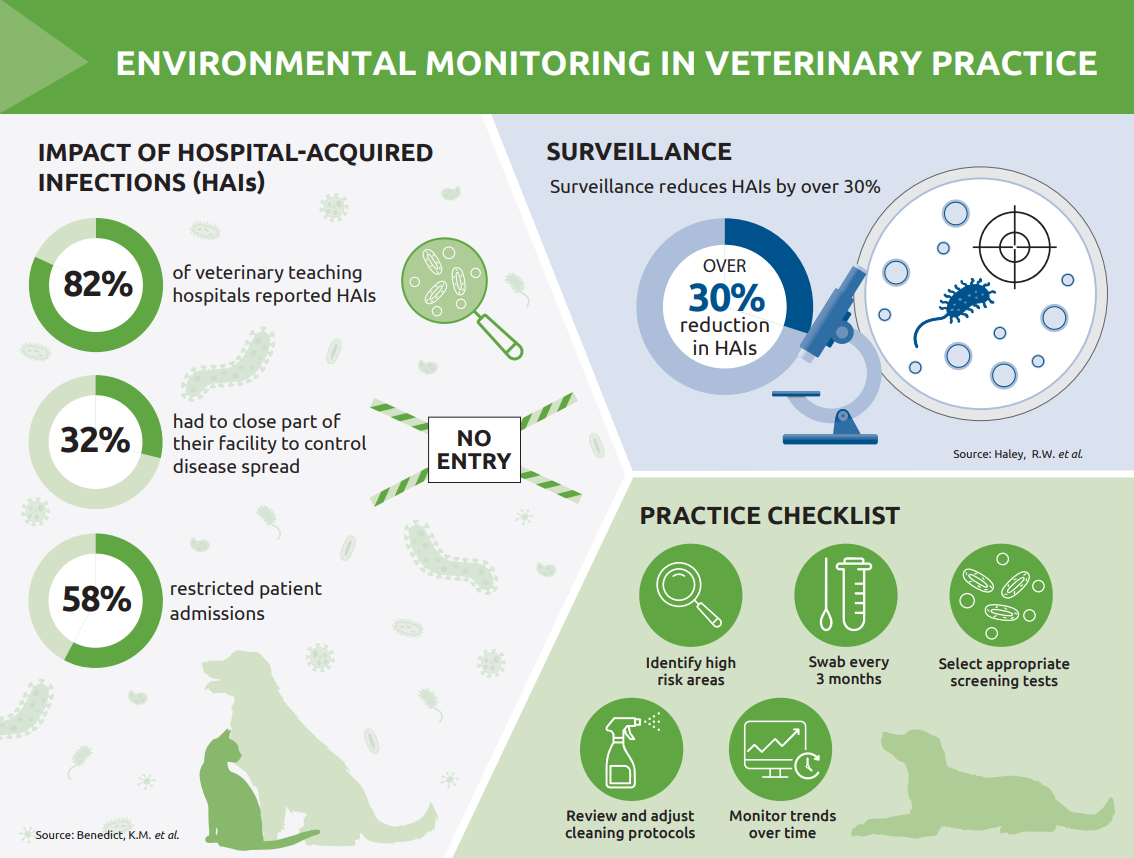
While equivalent data is lacking in veterinary medicine, in one study, 82 percent of veterinary teaching hospitals reported HAIs over a five year period.1 And while HAIs have consequences for the individual patient, they may also have a wider impact. Thirty two percent of the teaching hospitals in the study had to close part or all of the facility to control disease spread, while another 58 percent had to restrict patient admissions. Rising rates of antimicrobial resistance mean that without a proactive approach, these figures are only likely to increase.
Hospital-acquired infections
HAIs in veterinary medicine encompass a range of pathogens, many of which are highly concerning due to antimicrobial and multi-drug resistance. Among the most notable are the so-called ESKAPE pathogens2:
- Enterococcus faecium
- Staphylococcus aureus
- Staphylococcus pseudintermedius
- Klebsiella pneumoniae
- Acinetobacter baumannii
- Pseudomonas aeruginosa
- Enterobacter spp.
These pathogens are particularly concerning due to their ability to evade antimicrobial treatment, making them a significant challenge in both veterinary and human healthcare. Many are multi-drug resistant, compounding the difficulty of managing infections effectively and increasing the potential for poor outcomes. As a result, they have been given ‘priority status’ by the World Health Organisation (WHO) and most are included in the WHO Bacterial Priority Pathogens List (BPPL) – a list of microorganisms against which new antibiotics are urgently needed.3
In addition to the ESKAPE pathogens, other common causes of HAIs in veterinary practiceinclude Clostridium species and Escherichia coli, both of which can cause severe gastrointestinal disease, especially in vulnerable patients.
What is the source of HAIs?
While the exact source of hospital-acquired infections is not always clear, environmental contamination is widely recognised as a major contributing factor. In veterinary settings, pathogens can persist on surfaces, equipment and in water systems, creating reservoirs of infection. These microbes may survive routine cleaning, particularly when biofilms – complex structures formed by certain bacteria such as Pseudomonas aeruginosa – are present.
Patients themselves can also act as sources of contamination, shedding pathogens that remain viable in the environment, on staff uniforms, bedding and other high-touch areas. Regular swabbing and microbiological screening of surfaces and equipment can help identify potential hotspots of contamination before they become a problem.
Why environmental surveillance matters
While thorough cleaning and disinfection are the cornerstone of infection control in veterinary settings, the question remains: how do you know your protocols are effective? Regular environmental monitoring provides the data needed to confirm that cleaning is effective and helps to identify potential risks before any impact on patients.
In human healthcare, programs that incorporate environmental monitoring or surveillance have been shown to reduce HAIs by over 30 percent.4 The same proactive approach is equally valuable in veterinary practices, helping to establish whether pathogens like Pseudomonas aeruginosa or Staphylococcus pseudintermedius are persisting despite cleaning and disinfection. As well as identifying any reservoirs of infection, environmental surveillance is also useful for investigating outbreaks, providing early warnings of infection risk and allowing timely interventions to prevent further spread.5
How to create an effective monitoring protocol
Developing a monitoring protocol does not have to be complex, but consistency is key. Begin by identifying high-risk zones within your practice, such as surgical suites, recovery areas, and isolation wards. From there, create a schedule for regular swabbing and testing of surfaces, equipment, and even air or water quality. Swabbing every three months is recommended, but frequency can be adjusted depending on requirements.
What should you screen for?
In addition to bacterial pathogens, screening may also include testing for the presence of yeasts and moulds, as these can also present risks especially in immunocompromised patients. A comprehensive screening package is likely to include Enterobacteriaceae, Clostridia spp., Pseudomonas spp., MRSA, yeasts and mould.
Enterobacteriaceae are especially useful for assessing general hygiene status. This group includes species that originate from the intestinal tract of animals and humans (as well as plants and the environment) and should be readily removed from equipment and surfaces by appropriate cleaning procedures. The presence of Enterobacteriaceae in high numbers signifies inadequate cleaning.
It is also worth noting that testing for Clostridia spp is particularly important. These gram-positive bacteria form spores that are extremely resistant, including to many disinfectants. The spores can therefore be very difficult to eradicate.
Make infection control a priority
Integrating environmental monitoring into practice protocols offers several benefits:
- Improved infection control: early detection of pathogens allows for early intervention and a reduced likelihood of HAIs.
- Support for antimicrobial stewardship: monitoring data can guide more judicious use of antimicrobials
- Protection for staff and clients: identifying zoonotic pathogens ensures a safer environment for everyone
The RCVS Practice Standards Scheme Modules reinforces the importance of a clean, well-maintained clinical environment. Furthermore, environmental swabbing of all clinical areas is a requirement of achieving hospital status and needs to be carried out in accordance with infection rate audits.
Environmental monitoring is not just a reactive tool for managing outbreaks – it is a proactive investment in the health and safety of both patients and staff. By integrating regular testing into your infection control protocols, your practice can meet the highest standards of cleanliness and care. Start 2025 with a commitment to a cleaner, safer future.
References
- Benedict, K.M. et al. (2008) Characteristics of biosecurity and infection control programs at veterinary teaching hospitals. AVMA Publications. 233(5)
- Oliveira, D. et al. (2020) Antimicrobial resistance in ESKAPE pathogens Clin Microbiol Rev 33 e00181-19 https://doi.org/10.1128/cmr.00181-19
- The World Health Organization (WHO) Bacterial Priority Pathogens List, 2024
- Haley, R.W. et al. (1985) The efficacy of infection surveillance and control programs in preventing nosocomial infections in US hospitals. Am J Epidemiol 121: 182–205. 10.1093/oxfordjournals.aje.a113990.e.a113988 [DOI] [PubMed] [Google Scholar
- Dorina Timofte, D. & Jepson, R. (2024) PRO: Environmental microbiological surveillance does support infection control in veterinary hospitals, JAC-Antimicrobial Resistance. 6:4 https://doi.org/10.1093/jacamr/dlae113
About the author
Michelle Pittilla – Head of Microbiology Department at NationWide Laboratories
BSc (Hons) Biomedical Science
Michelle graduated with a BSc (Hons) in Biomedical Science from the University of Central Lancashire. With a strong background in clinical microbiology, she leads her team in ensuring that patient and environmental samples meet safety standards. Passionate about infection control, Michelle enjoys sharing her knowledge to try and enhance understanding of hygiene practices in veterinary settings. Her hands-on experience and commitment to improving client outcomes make her a trusted voice on the importance of environmental monitoring in veterinary practice.
Original publication: Veterinary Edge, issue 47, January 2025, pp 24-25