Canine pyoderma: a common dermatological challenge
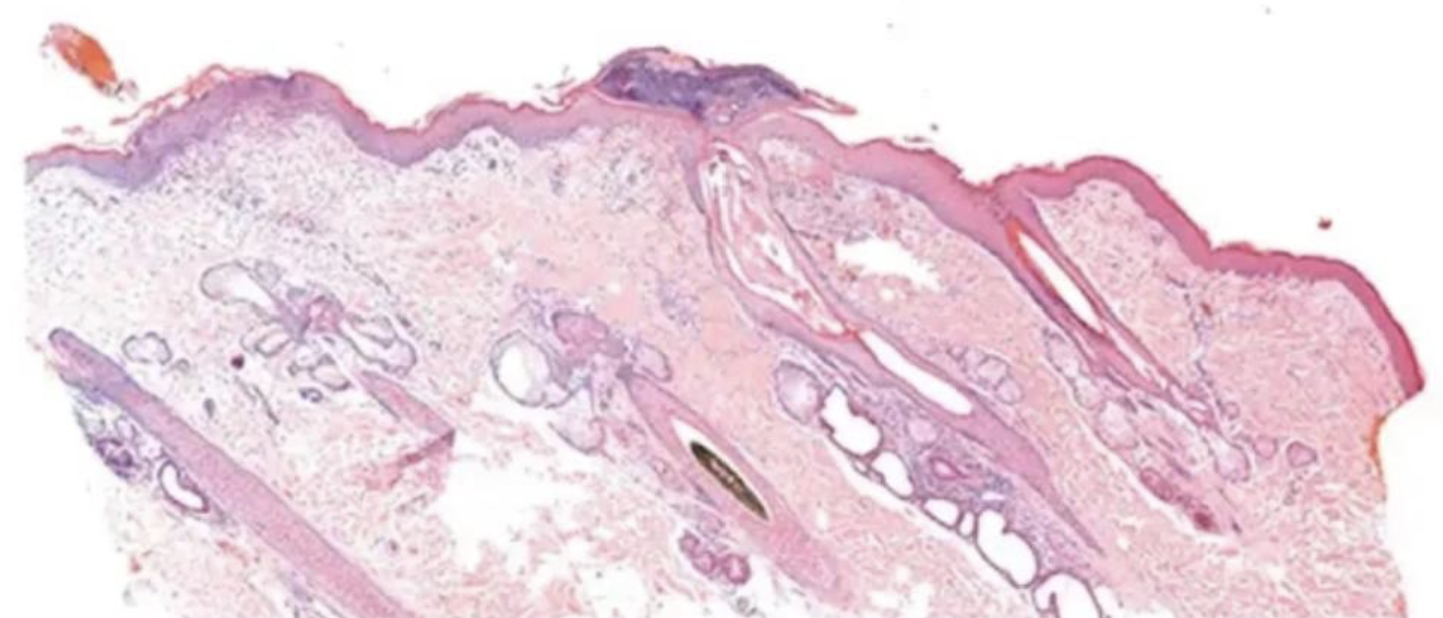
Figure 1. Skin. Superficial pyoderma. Focal pustule and superficial dermal chronic active inflammation.
Author: Karina Fresneda
Canine pyoderma is a common bacterial skin infection predominantly caused by Staphylococcus pseudintermedius. Depending on the depth of infection, pyoderma can be classified as surface, superficial and deep (Table 1).
Lesion location and total area affected varies between patients and the specific type of pyoderma present. Each type of pyoderma can also be categorised as primary or secondary, the latter being most common.
| Surface | Superficial | Deep |
| Pyotraumatic dermatitis | Bacterial folliculitis | Deep folliculitis |
| Skin fold dermatitis | Superficial spreading pyoderma | Furunculosis |
| Bacterial overgrowth syndrome | Impetigo (puppy pyoderma) | Cellulitis |
| Mucocutaneous pyoderma | Lick granuloma |
Table 1. Summary of the different types of surface, superficial and deep canine pyodermas
Laboratory testing plays an essential role in differentiating other conditions from canine pyoderma, identifying underlying comorbidities in secondary cases, and determining which antimicrobials are effective against the infection.
With up to 92% of cases being prescribed systemic antimicrobial therapy (Summers et al, 2014) and the recent emergence of meticillin-resistant Staphylococcus pseudintermedius (MRSP; Bloom, 2014), an accurate diagnosis of canine pyoderma has become imperative for effective treatment and preventing antibiotic resistance.
Pathogenesis
Pyoderma is caused by a bacterial infection of the skin which causes an inflammatory reaction. The most common bacteria implicated in canine pyoderma is S pseudintermedius, which is a normal commensal bacterium of the skin.
Canine skin can become infected with other Staphylococcus species such as S schleiferi, and other bacteria such as Escherichia coli and Pseudomonas aeruginosa, but this is less common (Bajwa, 2016). The depth of infection determines the classification for canine pyoderma (Figures 1 to 4).
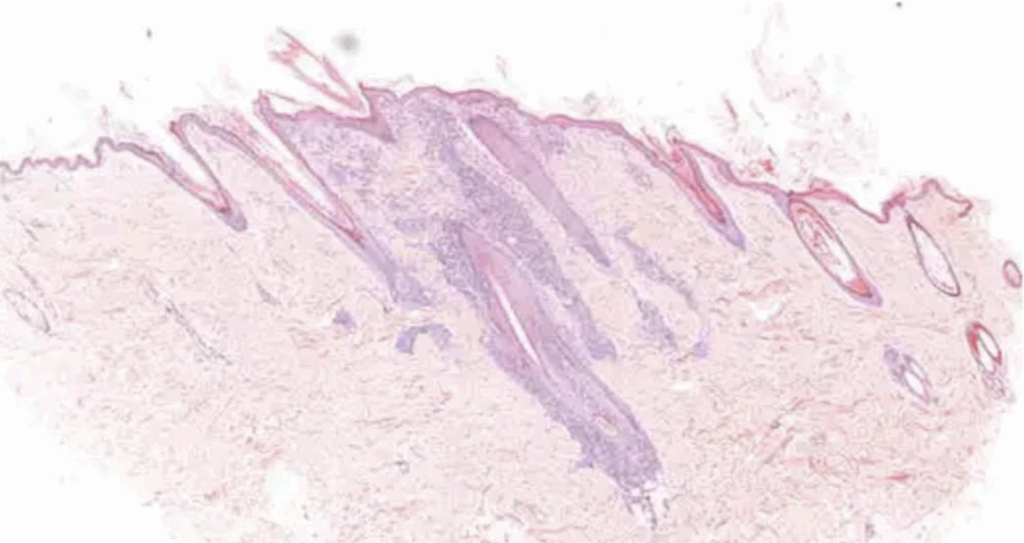
Figure 2. Skin. Superficial pyoderma and perifolliculitis. Superficial dermal chronic active inflammation, including perifollicular space.
Surface pyoderma is limited to the epidermis. Superficial pyoderma affects the epidermal layer of the skin, as well as the hair follicles.
Deep pyoderma involves the dermis, subcutis and hair follicles, and has the potential to cause a systemic bacteraemia. Demodicosis is commonly associated with deep pyoderma infections in dogs (O’Neill et al, 2020).
Primary canine pyoderma is seen less frequently and develops because of bacterial overgrowth on the skin, despite otherwise healthy skin (Tait, 2021).
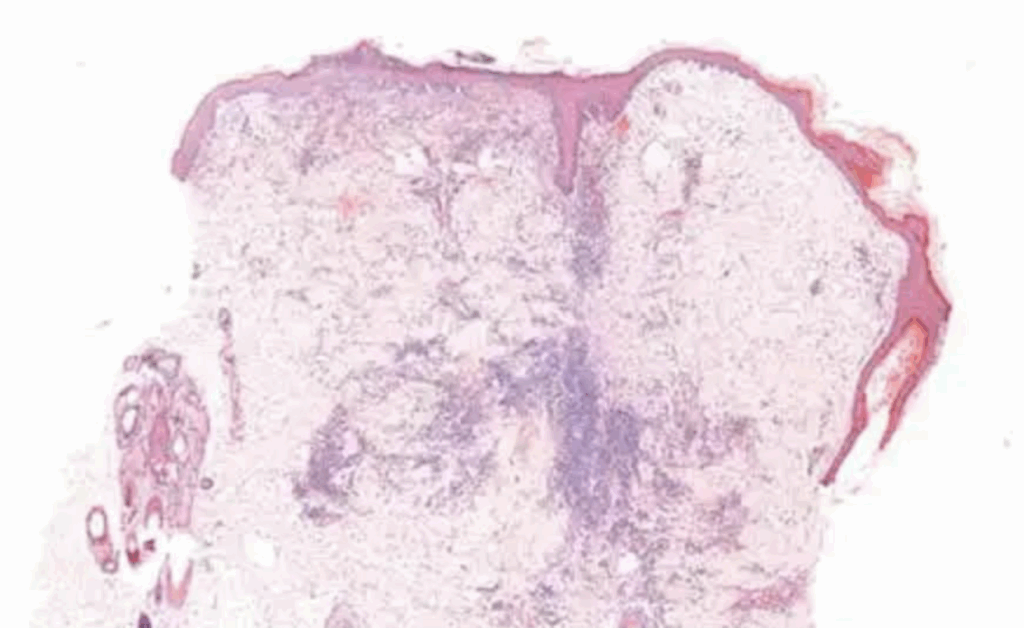
Figure 3. Skin. Superficial and deep pyoderma, superficial and deep dermal chronic active inflammation.
Primary pyoderma is predominantly seen in immunocompromised patients. Meanwhile, secondary canine pyoderma is far more common, yet complex. Underlying pathologies interfere with the skin’s normal integrity and function, damaging the protective barrier.
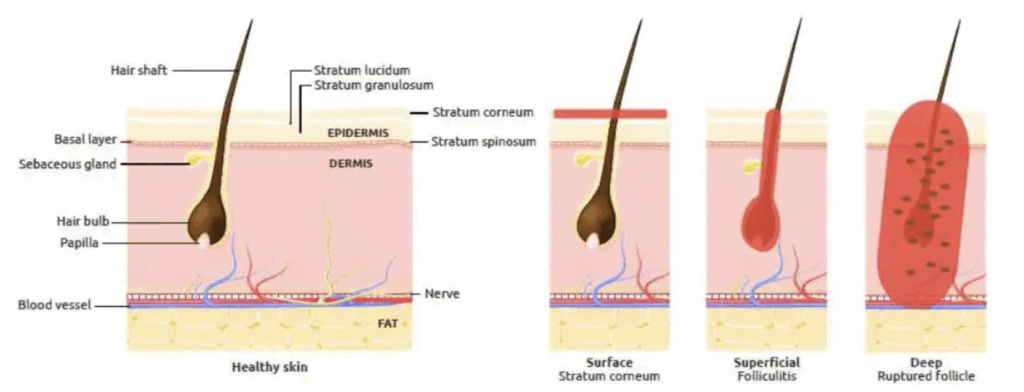
Figure 4. Classification of canine pyoderma based on depth of infection (Tait, 2021).
Some of the common underlying causes include:
- Ectoparasites – demodicosis
- Allergic disease – atopic dermatitis, food allergies and flea allergic dermatitis.
- Poor grooming.
- Follicular dysplasias.
- Keratinisation disorders.
- Endocrine disease – hypothyroidism and hyperadrenocorticism.
Any condition that damages the skin barrier allows commensal bacteria to penetrate the skin, proliferate and elicit an inflammatory response. This results in a secondary bacterial infection
(Tait, 2021). Damage to the skin barrier can either be intrinsic or through excoriation due to pruritus.
Clinical signs
Several dermatological lesions are associated with canine pyoderma. The lesions present will vary slightly depending on the classification of pyoderma and the severity of the patient’s condition. Surface pyoderma classically features erythematous, moist, ulcerated lesions with areas of alopecia.
Papules, pustules, crusts and epidermal collarettes are commonly seen in cases of superficial pyoderma. Recurring canine pyoderma may lead to chronic changes to the skin, such as lichenification and hyperpigmentation.
Deep pyoderma is more painful and features furuncles, nodules, haemorrhagic bullae and sinus tracts. Bacteraemia caused by deep pyoderma would result in systemic signs, such as pyrexia, anorexia, lethargy and sepsis.
Pruritus is variable depending on the exact type of canine pyoderma present.
Differential diagnosis
Many of the lesions mentioned previously are also seen in other dermatological, autoimmune and endocrine diseases (Table 2).
| Differential disease | Overlapping lesions with pyoderma |
| Pemphigus foliaceus | Pustules, crusting, alopecia and epidermal collarettes |
| Dermatophytosis | Alopecia, scaling and crusting |
| Malassezia dermatitis | Erythema and scaling |
| Cutaneous lupus | Ulcers, scaling and crusting at mucocutaneous junctions |
| Atopic dermatitis | Erythema and pustules |
| Hypothyroidism | Alopecia and scaling |
| Cushing’s disease | Alopecia |
Table 2. Comparison of lesions in canine pyoderma and common differential diagnoses
Ideally, a diagnosis of canine pyoderma should not be made based on clinical signs alone. The similarity in lesion presentation among these conditions highlights the need for additional diagnostic tests to accurately differentiate between them.
The article continues beyond this point.
Read the full article https://www.vettimes.com/clinical/small-animal/canine-pyoderma-a-common-dermatological-challenge
Original publication: Vet Times (2025), Volume 55, Issue 22, Pages 6-14
About the author
Karina Fresneda, DVM DiplACVP is a veterinary pathologist at NationWide Laboratories, specialising in cytology and histopathology. A Diplomate of the American College of Veterinary Pathology, she brings international training and over 15 years of experience in diagnostics and teaching. Her expertise supports accurate interpretation of complex cases such as canine pyoderma.
More information on diagnostic approaches, pathology insights, and case interpretation is available in NationWide Laboratories’ Lab Facts handbook, created by our expert veterinary pathologists https://nwlabs.co.uk/lab-facts